Pneumonia
Coming soon…
Asthma
Unveiling the COVID-19 risks in Asthma Patients!
Since the day we were hit by the pandemic, there had been a lot of questions about this unknown VIRUS that was progressing in the world. The base of a lot of questions was ‘who all can be affected by it’. After research and a lot of studies, it was found that the VIRUS can hit anybody irrespective of gender or age. But one thing that came into focus was that the people who have co-morbidities i.e. the ones who have any pre-complications are at higher risk than the others.
Amongst this the one pre-condition on which there had been a lot of studies is Asthma.
Because both COVID-19 and Asthma affect lungs it is believed that they are correlated. When the pandemic had just hit the world, it was thought that asthmatic people will get affected largely but it is now found that such patients were not at higher threat to the disease, risk is equal as for non-asthmatics. There is no evidence that having asthma means increased risk to have the virus.
However, if an asthmatic patient was infected with COVID-19, then there is a need for them to be extra cautious. For instance, a person who has uncontrolled asthma might show severe symptoms but again these are not such which cannot be controlled.
Asthmatic people who have been tested positive for COVID-19 should follow the same protocols as others. They should be just extra careful of the hygiene and clean environment. For this, they need to keep their hands clean, wash them frequently with soap, and do use alcohol-based hand sanitizer. Keep your surroundings clean and keep disinfecting the room you are in.
During the researches being conducted, a fact that came ahead is that the asthmatic patients who use inhalers are at very low risk of infection than others. One possible explanation for this can be that the treatment been taken by asthmatic patients limits the ability of COVID-19 to attach to the lungs and reduce the inflammation too.
As it is now clear that asthmatic patients are less likely to be infected with the virus, the question that now arises is whether this principle applies to all types of asthma? Or do different types involve different risks?
Normally there are two types of asthma: Allergic & Non-Allergic.
While allergic asthma flares up with exposure to pollen and mold, non-allergic asthma is exacerbated by exercise, stress, cold weather, etc.
The studies have suggested that non-allergic asthma might lead to severe disease but no conclusive evidence has been found.
In the end, would just like to add that even though asthma does not carry high-risk factors to be infected with COVID-19 yet, prevention is always better than cure. Follow all the protocols as listed by the government such as wear a mask, keep away from crowded places, maintain a distance of 6 ft while communicating.
Also, since our country has started the largest vaccination drive, we urge you to go get yourself vaccinated. It is completely safe. There are no special concerns regarding side effects to vaccination in asthmatics. Asthmatic patients shouldn’t be scared of vaccination and side effects related to it.
Common Queries about Asthma
COPD
Coming soon…
Pleural Effusion
Coming soon…
Tuberculosis
Tuberculosis- The clock is Ticking
Tuberculosis, Rajaykshma or Kshya rog, is an ongoing menace even in 21st century. Greeks named it as “phthisis” which literally means to rot, decay or putrefy. In the year 1882, 24 march German microbiologist Dr Robert Koch announced the discovery of causative bacteria. Since 1995 WHO started commemorating this day to emphasize public health challenge due to tuberculosis. In 2015, WHO recognized TB as global epidemic and major health concern clamming millions of lives every year. Therefore came up with “End TB” program”. Proposing 95% reduction in deaths due to TB by 2035, 90% reduction in TB incidence and Zero-TB affected families facing catastrophic treatment cost by 2035.
In our country the burden has been enormous and to address the problem we have a national health program to focus on TB since 1962. IN 1997 it was renamed to RNTCP as Revised national tuberculosis Program simultaneously revising the strategy to combat TB. In 2020 govt. of India re-organized this to NTEP national TB elimination program to achieve “End-TB targets “ 5 year earlier to WHO time-line.
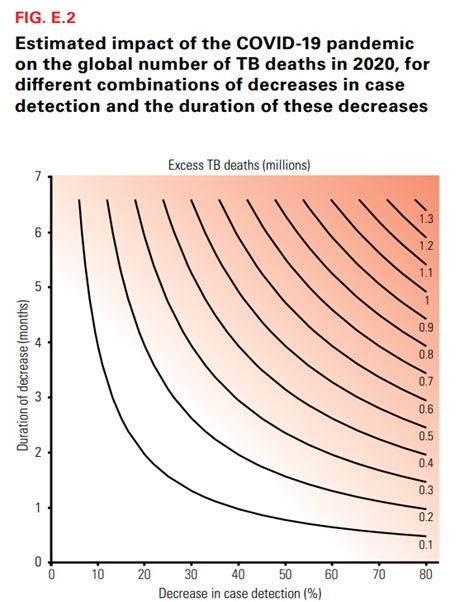
With emergence of HIV infection, lead to tuberculosis re-emergence, a difficult scenario to treat. IN the year 2020 world saw new pandemic of COVID-19 SARS-2 . This led to global lock-down bringing down the entire world, public health and economies to lowest nadir. This has affected drastically to public health program for Tuberculosis also. According to an estimation through modelling work a 25 % reduction in TB detection during lockdown due to COVID pandemic, would cause 4million excess deaths due to TB. COVID-pandemic threatens to unwind all efforts and achievements to control TB in last few years.
COVID-Pandemic led to:
Reduced reporting and case detection
Mobilization of health workers to COVID-care from TB program
Fund transfer from TB program to Pandemic care
GeneXpert and lab-machines utilized for COVID rather than TB
Access to TB drugs effected
Stigma of TB complexed with Stigma of COVID led to further lowering case-detection.
In resource -poor countries like ours , practically all major health care resources were diverted to control Pandemic compromising other health programs. This might put us back in achieving End-TB-Goals”
TB is still one of the top 10 causes of death worldwide. Despite the fact that it is a curable and preventable disease , it is estimated that 10 million people fell ill due to TB and almost 1.2 million lost their life to TB globally in 2019.An additional 2lac people died of HIV-TB dual infection. India accounts for ¼ cases of TB cases globally and of all MDR/R-R TB 27 % cases are from our country (this is highest in world).
Remember, TB is curable and preventable disease therefore if diagnosed early and properly managed lives can be saved and so are families , economies. Stigmatizing and hiding such disease would prove to be havoc. Same stands true for COVID disease. Despite all odds, Government is committed to public health goals and entire treatment is available free at DOTS -centers, DOTS-Plus centers and govt. hospitals.
Fact to remind, TB can affect any body system like brain , meninges, eyes, skin, Pulmonary, Pericardial ,pituitary gland, Lymph nodes, larynx or voice box, abdominal TB, TB of genital organs, Urinary tract, TB of prostate, testicular TB etc. Low fever, cough, weight loss, loss of appetite are common symptoms and other symptoms can vary according to organ involvement. At times patient may deny any symptoms. Genital TB might present with infertility.
Symptomatology, radiology or Imaging might be misleading and therefore evaluation of each and every case is must. Cure will certainly depend upon definitive diagnosis. Many diseases might mimic like TB and even cancer can present like Tuberculosis.
Diabetes, HIV, poor nutrition, are risk factors for developing tuberculosis. Other causes like over crowding , poor hygiene and sanitation, ill treated cases, not following Cough protocols lead to spread of infection.
During lock-down , social distancing and face-mask usages have helped breaking the transmission chain of Tuberculosis too. In fact all respiratory infections were cut down.
Clock-is Ticking, time is on the move and so is Tuberculosis. While you read this people are getting infected, falling sick to this microscopic monster, lives are lost due to this pre-puranic microbial disease even in mars mission age. Wake-up , know your enemy, enemy of healthy human life and society, combat at all level. The fight is not of any individual or the Government but for every one of us.
Foremost step, Stop coughing and spitting openly. Our ex-president and missile- man late shri APJ kalam said once, “ my country is my home” and we should not litter or spit in public places, its not a garbage box. Single step can significantly cut down spread of TB.
Lung Cancer
Cancer, is word which as a diagnosis can turn any one’s life upside down. Unfortunately, this dreaded disease is becoming more and more rampant.
As per 2018 WHO data an estimated 9.6 million deaths occur due to cancer globally. Approximately 70% of deaths from cancer occur in low- and middle-income countries. Cancer in one of the top five causes of mortality. Among all causes, Lung cancer is the commonest of all as well it is one of the most fatal one. Surprisingly, the incidence is rising among non-smoker and female population. Not only lung cancer, cancer of breast, colo-rectum , stomach, liver and prostate are also rising . Despite of strict regulations on tobacco use and trades, cancer especially lung cancer is rising. Environmental pollution is one of the most vital cause leading to rise in various respiratory diseases including Cancer.
Ambient air pollution is new age monster, claiming a large number of human lives. Air pollution kills an estimated seven million people worldwide every year. WHO data shows that 9 out of 10 people breathe air which would be graded as polluted as per air qulity standards. Majority of the affected are from third world countries and most poor of the people. Air pollution is responsible for nasal allergies, burning eyes, worsening of asthma, COPD, Coronary artery disease, Brain strokes, Stress, traffic accidents secondary to poor visibility and cancers. Most drastically the children have higher health risk due to pollution. Even Foetus inside the womb is not safe from pollution and PM2.5 or PM1 can cross placental barrier and lead to growth retardation. Not only lung cancer but various other cancer have been linked to pollution exposure like breast, colon, pancreas and liver. (American association of cancer research ) A study by the International Agency for Research on Cancer (IARC) determined that there is enough evidence to say that outdoor air pollution can cause cancer in people. This report also specifically implicated PM2.5
Apart from Particulate matter (PM10, 2.5, and PM1) various oxides and aromatic fumes are also carcinogenic. Air pollution contains several mutagens and carcinogens, including PAHs (eg, benzo[a]pyrene and polar compounds),dioxins, sulphur‐containing compounds (SO3, H2SO4), and 3‐nitrobenzanthrone. These Polycyclic aromatic hydrocarbons (PAHs) can alter the host DNA , overwhelming the repair capacity. Polycyclic aromatic hydrocarbons (PAHs) are a class of chemicals that occur naturally in coal, crude oil, and gasoline. They also are produced when coal, oil, gas, wood, garbage, and tobacco are burned. Tobacco and nicotine are very highly associated with cancer. Even second-hand smoking has contributed to development of asthma, worsening COPD, and various cancers.
Ambient air pollution is modifiable risk factor for cancer. This is also compounded by indoor pollution attributed by bio-fuel, cooking, wood burning, poor ventilation, cleaning chemicals and aerosols. It sounds like for all the development and industrialization we are paying a huge price by compromising with air quality and our health. Medical advancement has given umpteenth drugs/chemotherapy, radiotherapy and surgeries to effectively manage the cancer menace and that’s the only ray of hope for people suffering from cancers. However, if we combat collectively against ambient pollution, we may be able to curtail on incidence of cancer and so many other diseases which are on the rise and claiming human lives and happiness. Its high time to think and act. Fight cancer fight pollution
One fight , hundred gains. If we can abolish pollution can definitively control Cancer, COPD,IHD, Stroke, and human suffering.
ILD (Pulmonary Fibrosis)
To understand, ILD is a condition where interstitium or skeletal of lung get fibrosed, thickened leading to Poor takeover of oxygen. Hence oxygen levels start to drop, more often with activity, walk or stair climbing. ILD is an umbrella term and has variety of reasons and outcomes. In a variant, the disease may be rapidly progressive leading to early crippling and death, however on the other extreme it may be very slowly progressive or even may respond to treatment so well that may regress. In all , there is no need to panic rather take a professional advice, start the proper treatment and follow up regularly to know the exact response to treatment and prognosis.
To ascertain the cause of ILD and extent of the disease many tests would be required. Routine blood test, HRCT Chest(high resolution cat scan), pulmonary function including diffusion capacity, walk test or oxygen desaturation test, work up for rheumatic disorders(CTD), HYPERSENSITIVITY PNEUMONITIS, exposure to organic dusts, occupational history all would be needed for a fresh case. Cardiac evaluation and extra-pulmonary systems would also be assessed in appropriate cases. Few of these tests might need to be repeated for response assessment. History of exposure to pets, birds, molds/funguses, damp surroundings, grain storage, industrial gases and chemicals, indoor plants all is important and should be shared with treating doctor. For some patients, lung biopsy might be needed. Lung -biopsy usually done by fiberoptic bronchoscopy +- cryo-probe. Some patients may be advised open lung biopsy/VATS biopsy.
PFT and six minute walk test are functional tests needed more often. Progressive cases would need oxygen supplementation at home. Controlling weight, smoking habit, coexistent asthma or any other ailment has to be treated well. Keeping the surroundings clean and free of air-pollution also partially helps. For drug management, steroids, immune-suppressants and anti-fibrotic medicines are frequently required. All these medicines do have serious side effects and therefore regular review and follow up is a necessity. Drug doses, steroid doses are gradually tapered down or titrated as per control of disease and symptoms. Other supportive drugs, nebulization or bronchodilators, cough suppressant, anti-oxidants/ vitamin supplements are prescribed. At times disease may progress despite of treatment as well there may be time to time variations and exacerbations causing unscheduled opd or emergency visits.
Post Covid Care
Coming soon…
Sleep Apnea (OSAHS)
Sleep is one of the most important physiological need. It’s the time of day when body recovers, cells and organ tissues repair the injury of day to day activity. Sleep might sound inactivity from voluntary work and task but physiologically its an active repair time. Therefore sleep is as important as day life for a normal healthy body and mind. Disturbances of sleep in long run can be dangerous and fatal. Abnormal sleep pattern or sleep disorders affect entire body.
Headache, chronic fatigue, poor memory, lack of concentration, day time lethargy/sleepiness, low appetite, obesity/ weight-gain, swelling, higher blood pressure, high blood sugars, heart diseases psychological disorders and even stroke are possible health effects of sleep disorders. Apart from medical issues it is a factor for road traffic accidents, social discard, broken marriage / ground for divorce and worsened professional performance.
Fortunately ,there are tests and treatment available for this syndrome. Syndrome because it brings many diseases together. However, the first step is to acknowledge the problem. Unfortunately majority of public would take it as a social problem of snoring and not considering a disease worth consulting . Denial is the major problem and secondly using CPAP machine as treatment is not well accepted by patients. Although, despite of several researches and advancements CPAP remains the most efficient treatment option.
In few cases of maxillofacial deformities, surgical procedures or dentoaplatal splints /adjuncts can be of help in other cases best management plan is positive pressure devices like CPAP.
for further information watch the Video :-
Wake up fresh
Obesity & Diseases
World Obesity Day 2022
“Everybody needs to Act”
Obesity is considered as variability in body structure or body weight among humans. Mostly linked to food and calorie intake. However now it’s time to understand that Obesity may be a disease. Being over weight is calculated as per body mass index a ratio calculated using height and weight for an individual. Ideal body mass index is 18.5 to 24.9. BMI of more than 25 is overweight, >30 is obesity and >35 is classified as Morbidly obese. Obesity can not be ignored and considered as single disease , rather it’s the harbinger of multiple ill health effects. Apart from being a target for body-shaming and social out cast there are organic disorders associated with obesity. To enumerate obesity is associated for the following disorders :-
Hypertension (high BP)
Diabetes
Coronary artery disease (heart diseases)
Dyslipidemia (lipid and cholesterol disorders)
Gallbladder stones and cholecystitis
Stroke
Sleep Apnoea
Breathing disorders (Obesity Hypoventilation & Restrictive lung disorder)
Cancers like breast, gall bladder, uterus
Generalized hyper-inflammation (high CRP and leptins)
Secondary depression (due to social discard & physical inabilities)
Bone & Joint stress
The list is ever expanding as more and ore research is finding obesity as causative to many other health disorders.
To understand the causes of Obesity? We enlist the factors; Genetic or familial cause is non-modifiable risk factor. Eating habits, over-eating , junk food, is surely a contributing factor. Sedentary life style, lack of physical activity, exercise is another reason. Diabetes is one of the reasons for obesity as well effect of obesity. Thyroid disorders , hypothyroidism also causes obesity. fat metabolism abnormality too contributes to increased weight. Controlled calory intake Diet changes and regular exercise is the best defense against obesity.
“Everybody needs to act”
that’s the motivating theme by World obesity federation for the year 2022.
Obesity is not a single disease , it’s a syndrome , metabolic syndrome predisposing an individual to several complications. Therefore recognize and act. Act to modify life style and fight obesity.
Consult doctor if you are facing breathing issues with obesity you might be suffering sleep Apnoea or obesity hypoventilation. Dietary advise to exercise regimen, hormonal treatment to bariatric surgery various medical helps are available for your fight against Obesity. Need to Act.
Dr Sharad Joshi, MD
EDARM,FCCP,FACP,FCCS
Associate Director Pulmonology
Max Superspeciality Hospital , Vaishali
Sarcoidosis
Sarcoidosis is a disease characterized by the collections of inflammatory cells (granulomas) in any part of your body — commonly the lungs and lymph nodes. But can also affect the eyes, skin, heart and other organs.
The cause of sarcoidosis is unknown
Experts think it results from the body’s immune response to an unknown substance may be infectious agents, chemicals, dust or a potential abnormal reaction to the body’s own proteins (self-proteins) could be responsible for the formation of granulomas
General symptoms • Fatigue / Fever • Swollen lymph nodes • Weight loss • Pain and swelling in joints, such as the ankles Symptoms may vary as per the involvement of body organs. At times patient may present with facial paralysis or hearing impairment, Visual disturbance.
Pulmonary Sarcoid would present with cough, fever and breathlessness or chest tightness. The disease can actually mimic Tuberculosis however nature and management of both the diseases is grossly different.
It’s not contagious
It’s not cancer,
sarcoidosis is not a type of cancer as few patients may be scared of, although the disease may predispose to certain malignancies especially Lymphoma however the incidence s very low.
Diagnosis: Chest xray, Contrast Chest CT would be needed, in certain patients’ Endobronchial ultrasound, EBUS- FNA will help establishing the diagnosis.
Serum ACE level, is not a diagnostic test for sarcoidosis
Biopsy is most definitive test to establish diagnosis
Treatment for sarcoid is available.
Treatment is simple and has to be taken under proper guidance .However the treatment may be prolonged and response to treatment is variable. Steroids may be needed in certain stages ; some other immunosuppressive meds might be needed.
Pulmonary Rehabilitation
## Can I exercise?
• How can I get in better shape?
• Can I do anything to improve my overall well-being?
Pulmonary rehabilitation (PR) can help answer these and other questions. Participating in a PR program will help decrease your shortness of breath and increase your ability to exercise. You may have heard that pulmonary rehabilitation is only for people with COPD (chronic obstructive pulmonary disease). We now know that people with other lung conditions such as pulmonary hypertension, interstitial lung disease, pre/ post-transplant, and cystic fibrosis can benefit as well.
# What is Pulmonary Rehabilitation?
Pulmonary rehabilitation is a program of education and exercise that helps you manage your breathing problem, increase your stamina (energy) and decrease your breathlessness. The education part of the program teaches you to be “in charge” of your breathing instead of your breathing being in charge of you. The exercise sessions are supervised by a Physiotherapist that prepares an exercise program just for you. The exercises start at a level that you can handle (some people start exercising while sitting and others on a treadmill). The amount of time you exercise will be increased in time and the level of difficulty will change based on your ability. As your muscles get stronger, you will exercise longer with less breathlessness and be less tired.
## How much time does a Pulmonary Rehabilitation Program take?
Most programs meet two to three times a week and programs can last 4 to 12 weeks or more. Because your Physiotherapist constantly monitors your progress and increasing your exercises as you are able, attending every session is important.
How will I know if Pulmonary Rehabilitation is right for me?
Your doctor will determine if you qualify for pulmonary rehabilitation by:
■ Evaluating your current state of health and lung function test results
■ Discussing your current activity level and your ability to do the things you want to do
■ Determining your willingness and ability to attend.
Pulmonary rehabilitation programs are limited in the number of people who can attend so that you get close supervision. You will be evaluated before you begin the program to make sure you do not have health issues that would limit your ability to join.
## What will I do in the exercise sessions?
You may not think that you can exercise when just walking across the room makes you breathless. There are however, standard exercises that have been found to work well for people with breathing problems. The type and amount of exercise you will do will depend on what you can do now and as you get stronger, your exercises will increase. Exercise sessions begin with stretching exercises or warm ups, followed by exercises for your arms and legs. Usually you will do both exercises to build your strength and exercises to build your endurance (stamina). To build your strength, generally weights and lifting devices are used. For endurance, activities might include walking on a treadmill or in a corridor and/or using a stationary cycle. The amount of time you exercise depends on what you can handle. After attending pulmonary rehabilitation, people are frequently amazed at how much they can exercise and how much less short of breath they experience.
## What happens after I finish a Pulmonary Rehabilitation program?
It is so very important that you continue to exercise after finishing your rehabilitation program or you will lose all of the benefits you have gained. Before you finish the pulmonary rehabilitation, your Physiotherapist will design for you a long-term plan of exercise for you. Many programs offer a “maintenance” plan so that you can continue to exercise with others with breathing problems.
